Checking the Orthosis’ Alignment
- Physical Exam
- Planning the Orthosis
- Model Technique
- Handing Over the Orthosis
- Maintenance
- Products in the Spotlight
- Downloads
FIOR & GENTZ
Gesellschaft für Entwicklung und Vertrieb von orthopädietechnischen Systemen mbH
Dorette-von-Stern-Straße 5
D-21337 Lüneburg
Tel.: +49 4131 24445-0
Fax: +49 4131 24445-57
E-Mail: info(at)fior-gentz.de
Beratung und Technischer Support
Checking the Orthosis’ Alignment
Using the example of an AFO with NEURO SWING System Ankle Joint
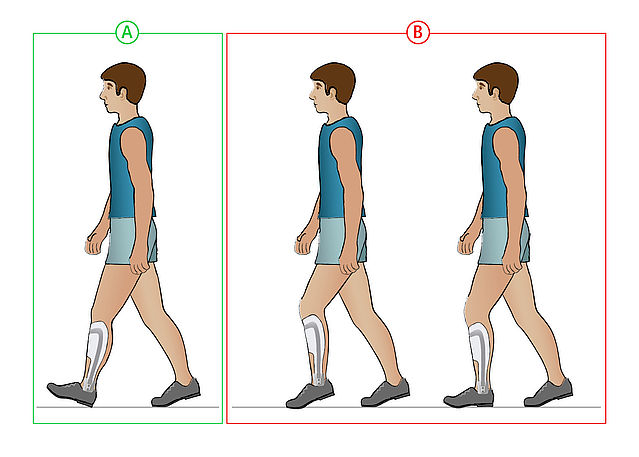
When handing over the orthosis to the patient, you check the orthosis‘ alignment, make adjustments and change settings, if necessary. The following construction serves as an example:
- AFO
- unilateral
- partially flexible foot piece
- NEURO SWING system ankle joint
In this online tutorial, we put our main focus on checking the alignment dynamically on the patient. It refers to unilaterally treated patients whose contralateral side is without restrictions. The AFO should be produced according to our treatment concept, which we illustrate in our online tutorials.
-
Preparations
-
Step 1/3
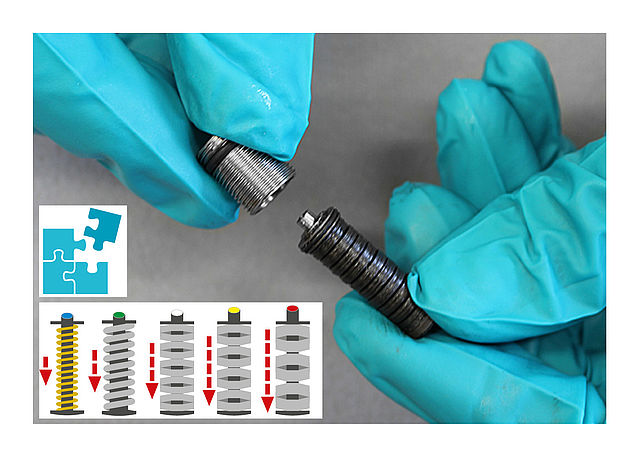
Mount the spring units (see also Joint Assembly NEURO SWING System Ankle Joint) according to the configuration recommendation.
Step 2/3
Check the position of the motion limiting screw inside the alignment screw:
A. motion limiting screw is unscrewed as much as possible → correct
B. motion limiting screw is not unscrewed as much as possible so that the spring’s range is limited → unscrew it as much as possibleStep 3/3

Mind the markings indicating the joint angle. Mount the spring units in such a way that the indicator is in the middle so that the alignment corresponds to the cast.



-
On the Workbench
-
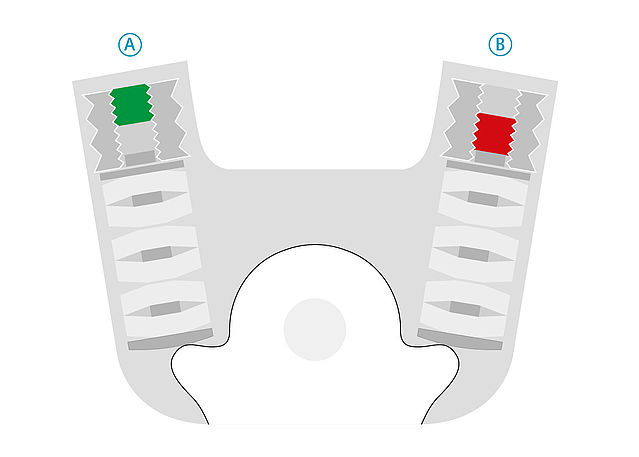
Step 1/1
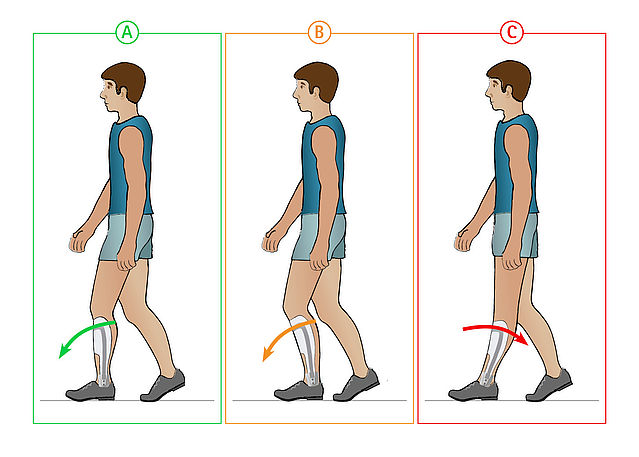
Check the alignment on the workbench considering the shoe pitch:
A. correct
B. tibia inclination too small → unscrew ventral spring unit until the alignment is correct, then turn the dorsal one until it has contact to the system stirrup again → check again
C. tibia inclination too high → unscrew dorsal spring unit, then screw in the ventral one until the alignment is correct; turn dorsal spring unit until it has contact to the system stirrup again → check again
-
Statically on the Patient
-
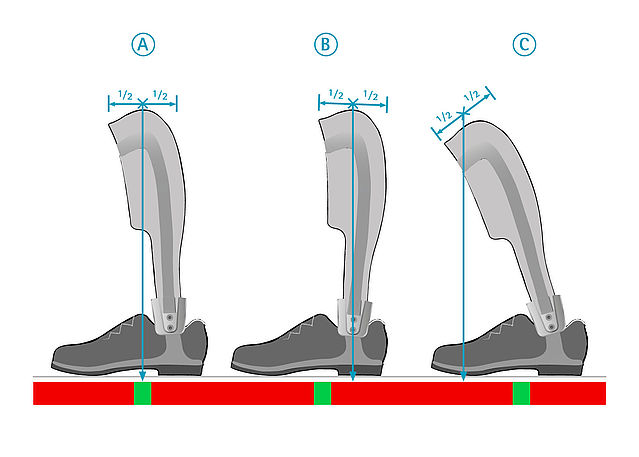
Step 1/1
Check the orthosis’ alignment on the patient, while the patient leans forward against the contact area:
A. patient is standing safely (with or without medical devices) and the plumb line falls into the green or yellow marked area → correct
B. patient needs help standing because he falls forward and the plumb line falls into the red marked area →- check settings and functionality of the medical device
- unscrew dorsal spring unit a little and screw in ventral one; make sure there is no play in the system joint and check again from the previous step (On the Workbench) → if the plumb line still falls into the red marked area: mount a stronger spring unit ventrally and leave the alignment as it is for now; check again
-
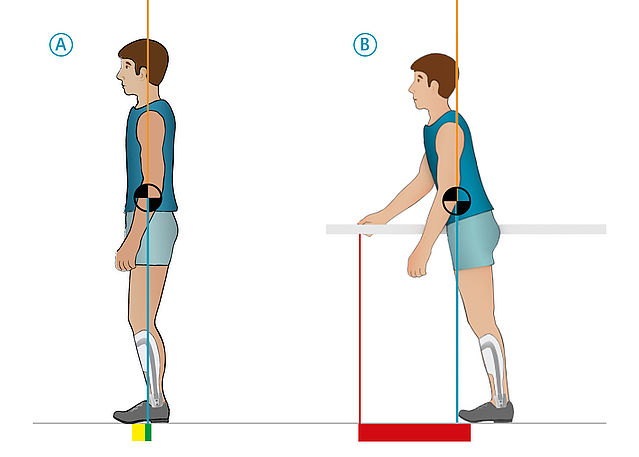
Dynamically on the Patient
-
Step 1/14
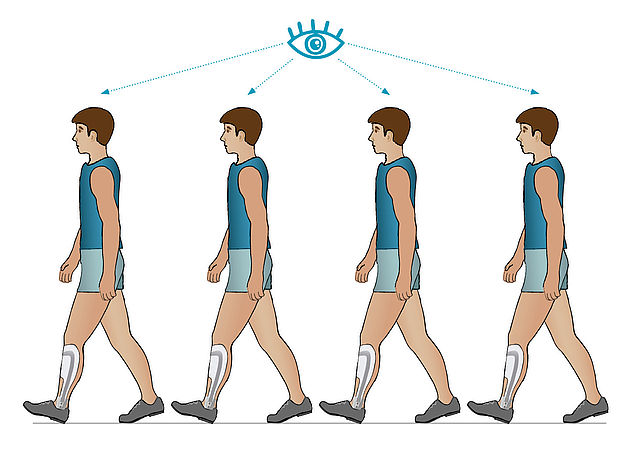
For checking the alignment dynamically on the patient, always examine several step processes.
Step 2/14
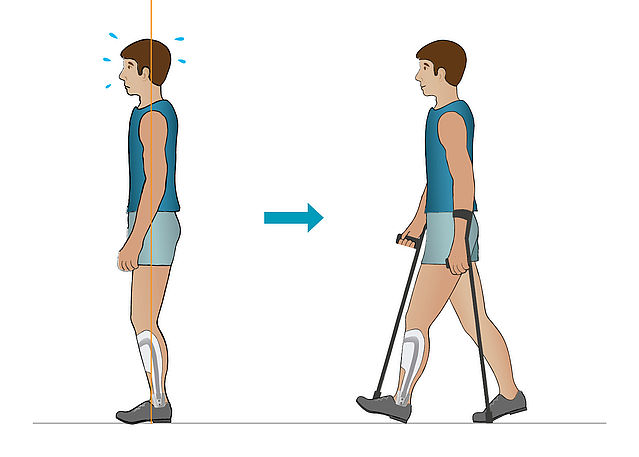
If the patient is still insecure, walking assistive devices can be used if necessary. Mind the correct settings, so that checking the alignment dynamically can be carried out successfully.
Step 3/14
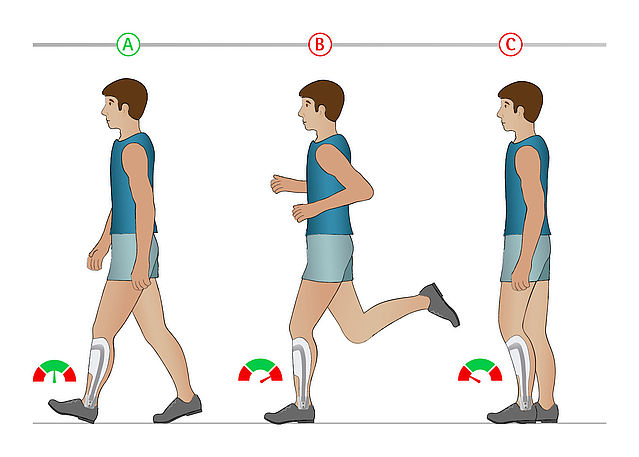
Check the walking speed*:
A. If it is about 84m/min (ca. 5km/h), the patient’s walking speed is normal and you can continue checking the alignment dynamically.
B. If it is about 200m/min (ca. 12km/h), it is not possible to check the alignment dynamically. Find cause (maybe the orthosis does not provide sufficient security).
C. If it is about 30m/min (ca. 1.8km/h), it is not possible anymore to identify the gait phases according to Perry reliably.
* Information about walking speed from: Götz-Neumann K (2011): Gehen verstehen – Ganganalyse in der Physiotherapie, 3rd edition. Stuttgart: Thieme, p. 19f.Note: You can also use the Timed Ten-Meter Walk Test (10MWT) to document the walking speed. (See: Tyler Klenow and Brian Kaluf: Timed Ten-Meter WalkTest (10MWT): Reference Guide. The American Association of Orthotists and Prosthetists, Outcomes Research Committee.)
Step 4/14
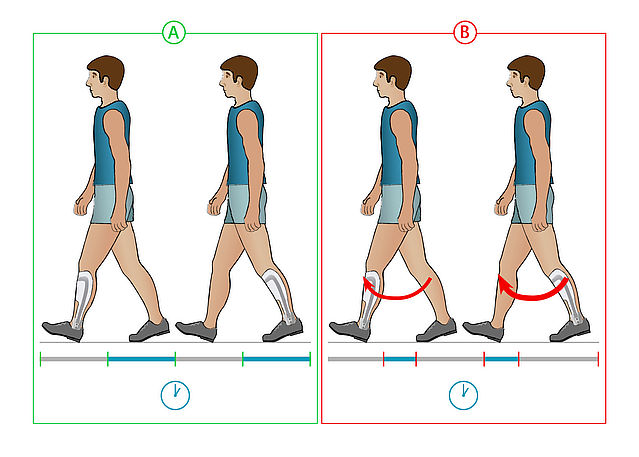
The load duration on both legs is:
A. the same → continue at the next step
B. not the same → find cause at the orthosis construction and resolve itStep 5/14
Initial Contact
A. initial contact with heel → correct; continue at step 8
B. initial contact not with heel → continue at step 7Step 6/14
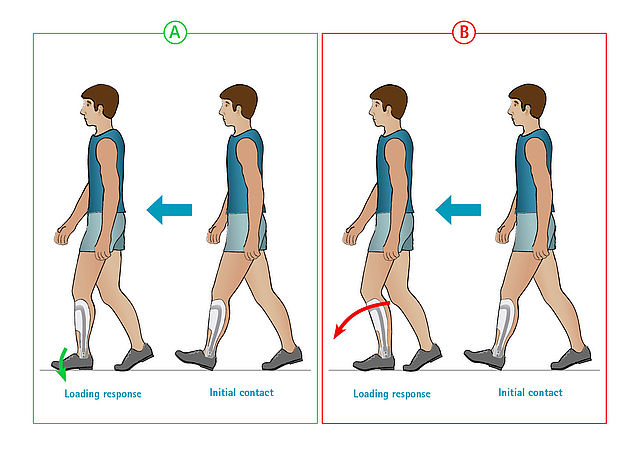
Initial Contact → Loading Response – Upper Ankle Joint
An initial heel strike occurs.
No → continue at step 8
Yes and
A. a plantar flexion occurs:- without noise when foot strikes the ground → continue at step 9
- with a loud noise (slapping) when foot strikes the ground → mount a stronger spring unit dorsally to control plantar flexion
B. no plantar flexion occurs (also noticeable by an increased knee flexion) → mount a weaker spring unit dorsally and check again until the situation under A. 1. is reached; continue at step 9
Step 7/14
Initial Contact → Mid Stance
Forefoot contact as initial ground contact and no heel strike even in mid stance.
A. No → continue at step 6
B. Yes. This is an active reaction of the patient to secure themselves → mount a stronger spring unit ventrally- successful: continue at step 8
- not successful: continue at step 6
- substructure under heel at the orthosis or, if necessary, the shoe until the initial contact occurs with the heel
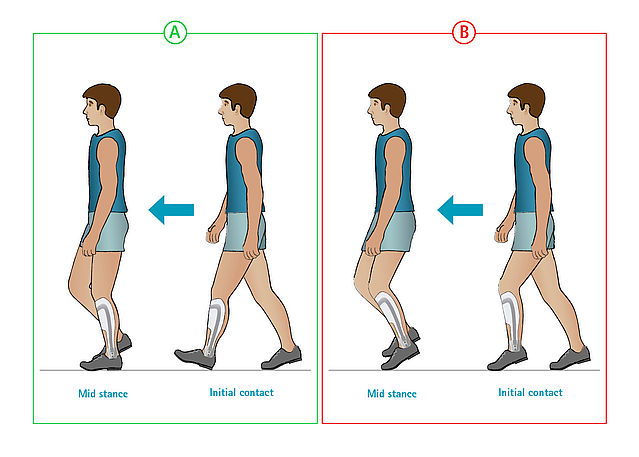
Step 8/14
Initial Contact → Mid Stance
A. complete foot contact or first contact with the forefoot and heel strike in mid stance
B. foot lifting is not sufficient in swing phase → mount a stronger spring unit dorsally- successful: continue at step 9
- not successful: substructure under heel at the orthosis or, if necessary, the shoe until the initial contact occurs with the heel
Step 9/14
Loading Response – Knee
A. knee is slightly flexed → correct; continue at step 11
B. knee is strongly flexed and there is (almost) no plantar flexion → patient does not allow sufficient plantar flexion; continue at step 10
C. knee is not flexed (maybe even hyperextended) → mount a stronger spring unit dorsally and check againStep 10/14
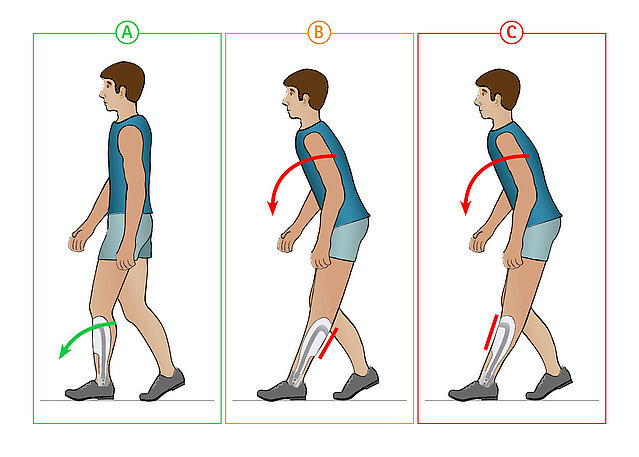
Loading Response – Knee
Knee is not flexed (maybe even hyperextended). Often, the patient bends forward the upper body in order to carry out a hyperextension despite the measures taken in step 9.
B. dorsal tibial shell:- produce new tibial shell with ventral contact area (ventral shell or appropriate cover)
- successful: continue at step 11
- not successful: continue at C. 2.
C. ventral tibial shell:
- check ventral contact area (shell or cover). It must be able to carry the load.
a. contact area is able to carry the load → correct; continue at C.2.
b. contact area is not able to carry the load → produce new tibial shell with ventral contact area (ventral shell or appropriate cover)
c. successful: continue at step 11
d. not successful: continue at C.2. 2. - mount a weaker spring unit dorsally
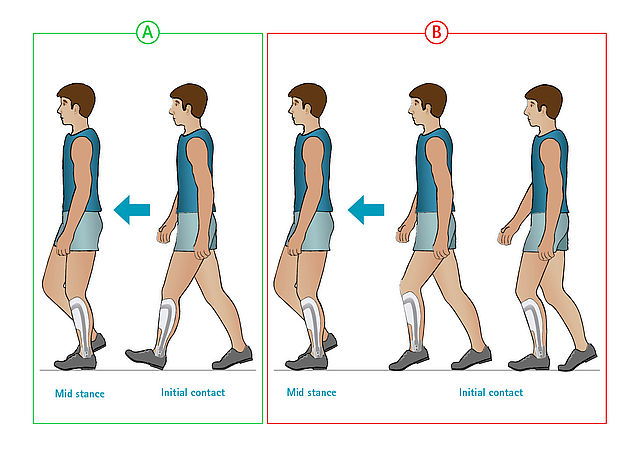
Step 11/14
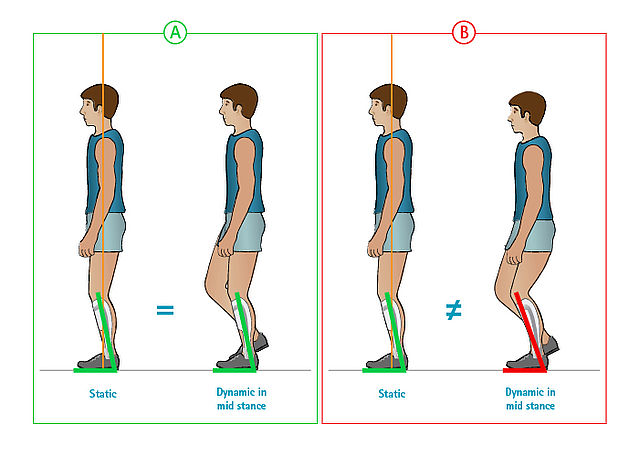
Mid Stance – Knee
A. tibia inclination corresponds to the one when the alignment was checked statically on the patient → correct
B. tibia inclination is higher than the one when the alignment was checked statically on the patient → mount a stronger spring unit ventrally. If the strongest spring force is not sufficient, screw in ventral motion limiting screw.Step 12/14
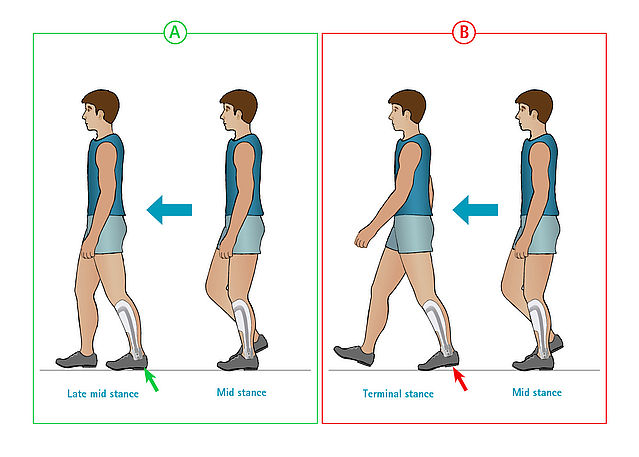
Mid Stance → Late Mid Stance – Ground Contact
A. foot contact is still complete and the contralateral side is in mid swing → continue at step 13
B. situation under A is skipped and the heel lifted immediately → mount a weaker spring unit ventrally; continue at step 13Step 13/14
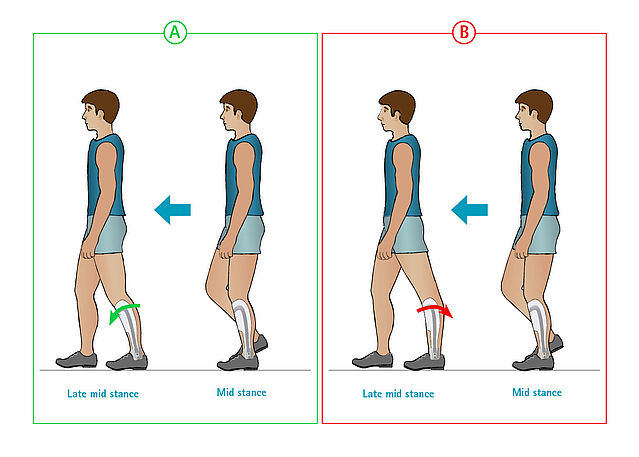
Mid Stance → Late Mid Stance – Upper Ankle Joint
A. tibia inclination increases (a dorsiflexion occurs)- without bumping noise → continue at step 14
- with clearly audible bumping noise → mount a stronger spring unit ventrally. If the strongest spring force is not sufficient, screw in ventral motion limiting screw and check again.
B. No dorsiflexion occurs (noticeable by a hyperextension).
- ventral spring unit is too weak and the patient secures themselves actively in hyperextension → mount a stronger spring unit ventrally; if necessary, screw in motion limiting screw and check again
- ventral spring unit is too strong and cannot be compressed so that a dorsiflexion is not possible → mount a weaker spring unit ventrally and check again
Step 14/14
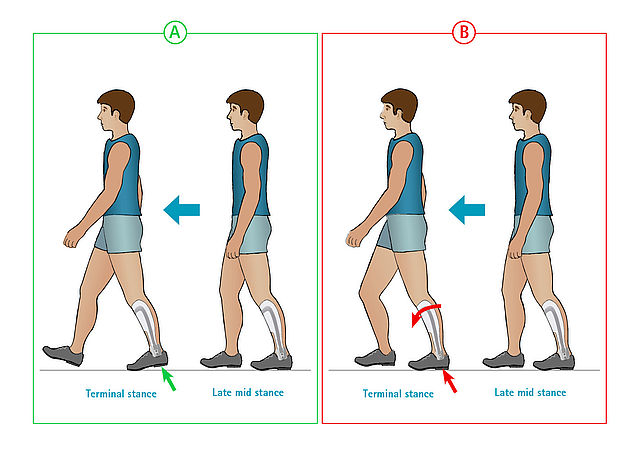
Terminal Stance
A. heel lifts significantly from the ground- without bumping noise à correct
- with clearly audible bumping noise → mount a stronger spring unit ventrally. If the strongest spring force is not sufficient, screw in ventral motion limiting screw.
B. heel does not lift from the ground → mount a stronger spring unit ventrally and, if necessary, screw in ventral motion limiting screw














Last Update: 20 March 2020
FIOR & GENTZ
Gesellschaft für Entwicklung und Vertrieb von orthopädietechnischen Systemen mbH
Dorette-von-Stern-Straße 5
D-21337 Lüneburg
Tel.: +49 4131 24445-0
Fax: +49 4131 24445-57
E-Mail: info(at)fior-gentz.de
Beratung und Technischer Support
